Partial knee replacements
If the damage in an arthritic knee is only affect one area or ‘compartment’ of the joint, then it is often possible to perform a partial knee replacement instead of a total.
As explained in furhter detail elsewhere on this site (CLICK HERE), we refer to the knee as having 3 separate compartments:
- the medial compartment is the articulation between the bottom end of the femur and the top end of the tibia on the inner side of the knee joint,
- the lateral compartment is similarly the articulation between the bottom end of the femur and the top end of the tibia on th outer side of the joint, and
- the patellofemoral compartment refers to the joint surfaces between the back of the kneecap (patella) and the V-shaped groove (the trochlear groove) that is present in the middle of the front and bottom ends of the femur.
If all 3 compartments of the knee are damaged, then the patient is likely to end up needing a total knee replacement, where all of the surfaces of the joint are resurfaced.
If the joint damage is only affecting the inner side of the knee, and if the rest of the knee is in good enough condition, then it might be more appropriate for some patients to have a medial unicompartmental partial knee replacement.
Likewise, if the damage is isolated just to the outer side of the knee, then it might be possible to have a lateral unicompartmental partial knee replacement.
What are the benefits of a partial replacement over a total?
Partial knee replacements tend to give better patient outcomes, with the following:
- a better post-operative range of motion of the knee,
- a partial replacement tends to give a joint that feels more normal (more like the patient’s own normal knee) compared to a total,
- they tend to give better functional outcomes, in terms of the kinds of activity that the patient is able to get back to, and
- they are associated with high patient satisfaction scores.

When is it NOT appropriate to have a partial replacement
It is important that patients are screened carefully prior to deciding to go ahead with a partial knee replacement, and the following are exclusions that would mean that a knee would not be suitable:
- the patient has a general propensity for more widespread primary osteoarthritis, affecting multiple joints,
- there is an inflammatory arthropathy, such as rheumatoid arthritis,
- the joint is unstable due to ligament ruptures / deficiency,
- if there is a significant fixed flexion in the knee (i.e. the knee does not go fully straight),
- if the joint is too stiff, with significantly restricted flexion, or
- if the arthritis is too advanced, and there is too much deformity (angluation) in the joint, especially if the deformity is fixed (i.e. not correctable).
If any of these exclusion criteria apply, then it’s simply better to have a total knee replacement instead.
What about the prosthetic survivorship figures?
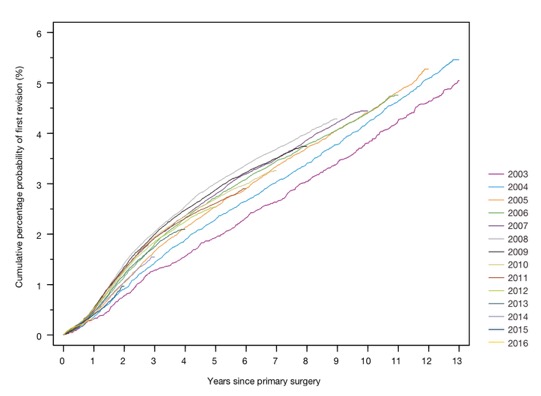
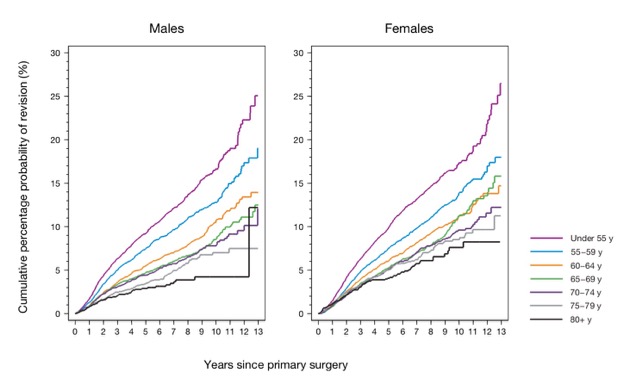
Approximately 95% of total knee replacements are still ‘in’ and working 10 years after implantation (i.e. only 5% will have ended up needing a re-do / revision within 10 years of the initial surgery).
The 10-year prosthetic survivorship figures for partial replacements are, however, lower than this…
With a partial replacement, approximately 10% of cases will need revision surgery within 10 years.
Another way of stating this is that the revision rate at 10-year follow-up for a partial replacement is double that of a total replacement!
However, there are some very clear and specific reasons for this:
- Partial knee replacements tend to be performed in younger fitter patients. The more active one is when one has a joint replacement, then the faster the rate of wear and tear will be on the artificial prosthesis, which simply means that it will wear out quicker – i.e. it will have a tendancy to fail sooner (compared to someone who is less active).
- In addition, the younger you are when you have a joint replacement, the longer you’re likely to live. This means more years of use and hence more years of wear and tear on the joint, and if a joint is eventually going to wear out at some stage, then the longer you live, the more likely it’ll be that this will actually happen within your lifetime.
- With a partial replacement, there is the risk that the wear and tear / arthritis may ‘spread’, and that you might at some stage end up developing arthritis in the other compartments of the knee, in which case you might then need the partial replacement converted (revised) to a total.
- Finally, it’s easier to revise a partial replacement than it is to revise a total. Therefore, surgeons’ thresholds for revision a partial replacement are lower than they would be for revising a total, and hence revision surgery is more likely to be considered for patients with partial replacements.
These factors are all important and all relevant; however, this does not mean that a partial replacement is ‘worse’ than a total – in many ways they are actually better… but only when done in the right patient at the right time for the right specific indications and reasons.
Types of partial replacement
The 4 main specific types of partial knee replacement are:
- a medial unicompartmental partial replacement
- a lateral unicompartmental partial replacement
- a patellofemoral replacement,
- a medial + patellofemoral or lateral + patellofemoral bicompartmental partial replacement and
- an Episealer focal resurfacing implant.
Medial / Lateral partial replacements
Excellent outcomes can be achieved with a medial or lateral partial knee replacement. However, it is important that the correct specific indications and the relevant exclusion criteria are followed carefully.
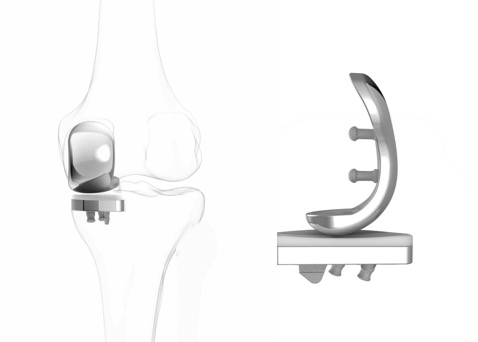
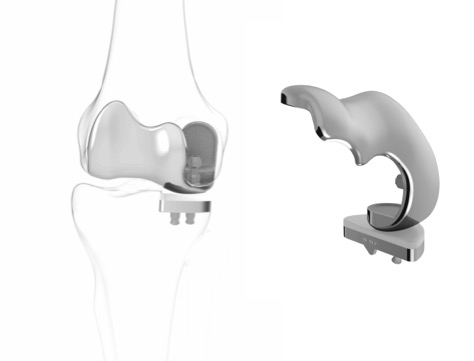
With a medial/lateral partial replacement, the surgery is performed through a smaller incision at the front of the knee, compared to a total. The surgery involves resurfacing either the medial or lateral compartment with metal prosthesis on the end of the femur and on the top of the tibia, which are both cemented to the surface of the bones, and there is a rock-hard plastic (ultra-molecular-weight polyethylene – UHMWPE) spacer in-between.
CLICK HERE to read the story of Kevin Budd – the first patient in the UK to have a Conformis iUni-G2 custom-made partial knee replacement.
CLICK HERE to read Helen’s story about what she achieved with her partial knee replacement.
CLICK HERE to read Anne’s story about her partial knee replacement surgery.
Bicompartmental partial knee replacements
In some relatively rarely cases, if there is damage in either the medial or lateral compartment, but also in the patellofemoral compartment too, if the patient is young and they have a high-functional demand, and if there is no evidence of any wear and tear / arthritis developing in the third ‘unaffected’ compartment, then it can sometimes be appropriate to use a bicompartmental partial knee replacement.
Is is incredibly hard to match the geometry of a medial or lateral compartment and the geometry of the patellofemoral comparment all at the same time, and some early designs of bicompartment replacement (like the Deuce knee) were associated with unacceptably high failure rates. However, a pretty much guaranteed fit can be achieved in both of the resurfaced compartments if a custom-made bicompartmental prosthesis is used, which is specifically designed (based on a high-res 3D CT scan of the patient’s knee) and then manufactured specifically for that individual patient, and this is achieved with the Conformis iDuo prosthesis.
Patellofemoral replacements

If the main medial and lateral weight-bearing surfaces in a knee are OK, but if there is isolated patellofemoral arthritis at the front of the joint (with bare bone on the back of the kneecap and/or over the trochlear groove at the front of the end of the femur), then a partial replacement with a patellofemoral prosthesis can give great results.
CLICK HERE to read more about patellofemoral partial knee replacement surgery.
The Episealer focal resurfacing implant

The Episealer is a small custom-made focal surfacing implant that is designed purely just for small focal full-thickness cartilage defects where the surrounding cartilage is in good condition and where the rest of the knee is fine.
CLICK HERE for further information about the Episealer.
How do I find out whether I might be a suitable candidate?
To find out whether or not you might potentially be a suitable candidate for a partial replacement rather than a total, you will need:
- a proper face-to-face assessment in clinic, including a detailed clinical examination,
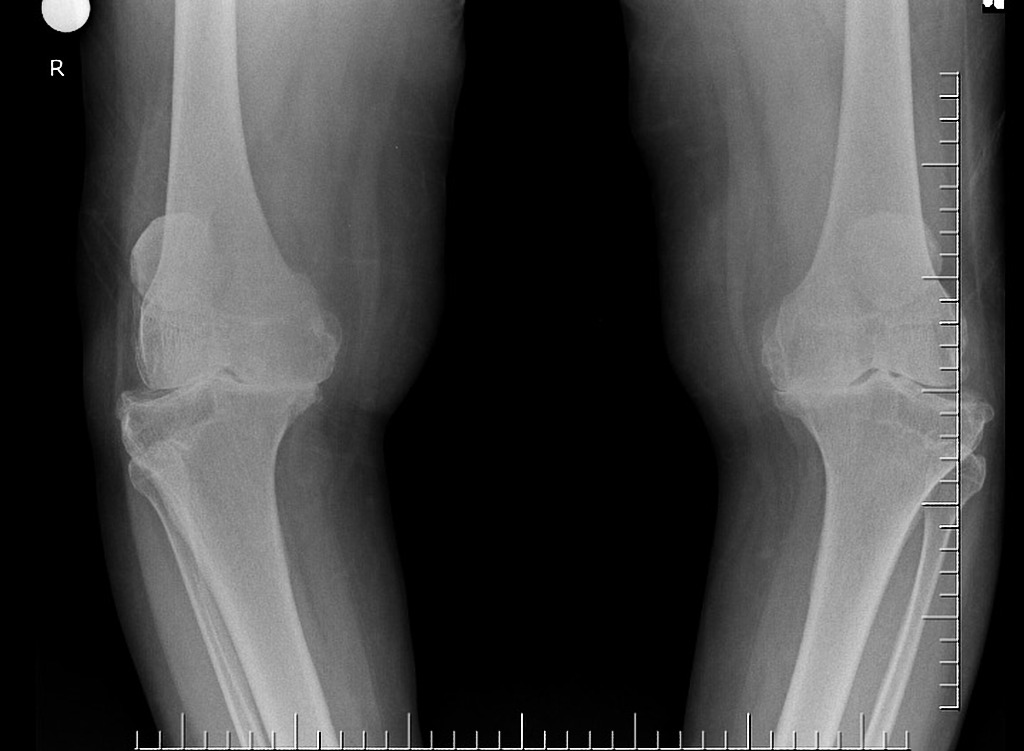
- a full set of up-to-date or recent X-rays of your knee (with a weight-bearing AP view, a Rosenberg /Schuss view, a lateral view, a patellar-skyline view and, potentially, also long-leg weight-bearing alignment X-rays), and most probably also a high-res MRI scan of the joint too (CLICK HERE to read about knee imaging), and
- a full, detailed comprehensive discussion with your surgeon about the pros, cons and risks of the surgery, along with a detailed discussion about the rehab and the likely outcomes.
- Sometimes it is also necessary / appropriate to perform a knee arthroscopy too, ahead of potentially proceeding with partial knee replacement surgery.
Book an assessment
CONTACT US if you would like to arrange an appointment with a full assessment of your knee.