Patellofemoral arthroplasty
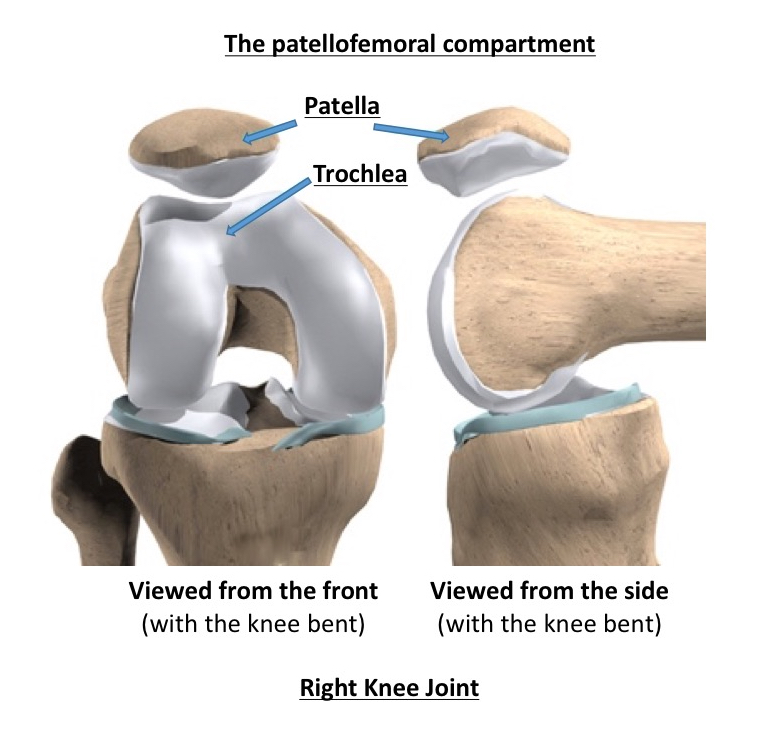
The term ‘the patellofemoral compartment’ refers to the articulation (the joint surfaces) between the back of the kneecap (the patella) and the V-shaped groove that sits in the front and bottom ends of the femur (the trochlear groove) at the front of the knee joint.
More often, arthritis tends to affect the whole of the knee joint (all 3 compartments). However, not too infrequently, the arthritic ‘wear and tear’ in a knee may only affect just the patellofemoral compartment, sparing the main weight-bearing surfaces between the femur and the tibia, i.e. the medial and lateral compartments. If the damage is limited to just the patellofemoral compartment, then we call this ‘patellofemoral arthritis’.
The symptoms of patellofemoral arthritis
The symptoms of patellofemoral arthritis are somewhat different from those of more widespread generalised osteoarthritis:
- people complain of pain at the front of their knee, around and behind the kneecap,
- most people are still relatively fine walking decent distances on flat even ground,
- with patellofemoral arthritis people have particular difficulty with activities that involve loading the knee with the knee in a bent position, e.g. going up or down stairs (especially down), squatting, kneeling or sitting with one’s knees bent for too long.

Why does patellofemoral arthritis occur?
Often, patellofemoral arthritis is just a genetic thing, and some people seem to be born with a natural predisposition. However, there are various issues that can pre-dispose specifically to patellofemoral arthritis, and these include:
- lateral patellar maltracking (where the kneecap sits off to the side instead of in the middle),
- patellar dysplasia (where the back of the kneecap is L-shaped for even flat, instead of the normal V-shape),
- patella alta (the kneecap sits too high up),
- patella baja (where the patellar tendon is too short, and the kneecap is too low down),
- patellar instability (particularly if there has been a history of multiple dislocations), or
- previous trauma to the front of the knee (e.g. fracture of the patella).
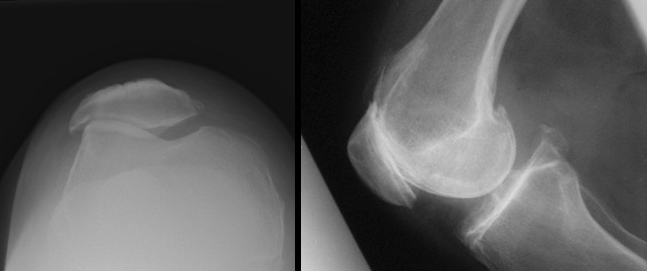
How do I tell if I do have patellofemoral arthritis?
Before deciding on any kind of potential treatment, and particularly any kind of actual surgical intervention, it is essential that you first get a full, detailed proper diagnosis. If you are suffering symptoms of knee arthritis and the pain is specifically around the front of your knee, and you’re questioning whether you might specifically have patellofemoral arthritis, and therefore be a potential candidate for a patellofemoral partial replacement rather than a total knee replacement… then you must seek an opinion from a specialist knee surgeon (one who can actually perform patellofemoral arthroplasty surgery!) and you must have proper detailed imaging of your knee. This should include:
- a full set of X-rays, including a weight-bearing AP view, a Schuss view, a lateral view and a patellar skyline view, and, importantly, also
- a high-res MRI scan of your knee too.
X-rays can only show you just so much, and hence an MRI scan is vital to check in detail what the condition of your medial and lateral compartments are, to ensure that the damage in the knee is actually isolated purely to just the patellofemoral compartment only.
How is a patellofemoral arthroplasty performed?
 The terms ‘knee replacement’ and ‘knee arthroplasty’ are interchangeable, and mean the same thing. Patellofemoral arthroplasty involves:
The terms ‘knee replacement’ and ‘knee arthroplasty’ are interchangeable, and mean the same thing. Patellofemoral arthroplasty involves:
- opening up the knee via an incision at the front of the joint (with an incision similar to but perhaps just slightly shorter than a total knee replacement incision),
- some of the bone (and whatever bits of cartilage might be left) off the back of the kneecap is ‘shaved’ away, giving a flat surface of fresh bone,
- some of the bone (and whatever remaining cartilage might be left) at the front of the femur is cut away,
- the back of the patella is then resurfaced with a rock-hard plastic (ultra-high molecular weight polyethylene – UHMWPE) ‘button’ that is cemented to the bone, and then
- the trochlear groove at the front of the femur is resurfaced with a metal prosthesis that is cemented in place.
The medial and lateral weight-bearing compartments and all of the knee ligaments are left alone and kept in place.
What are the results and outcomes?
A study from Sisto and Sarin from Camarillo, U.S., presented at the 2011 Orthopaedic Research Society Meeting, showed that:
- of 25 patellofemoral arthroplasties performed, with a follow-up of over 11 years, none had needed to be revised,
- all patients reported that they were ‘very satisfied’ with the prosthesis,
- there were no reports of weakness, instability or additional surgery, and
- all patients reported that they would undergo the surgery again.
CLICK HERE to read the full study.
Find out more...
CLICK HERE to read Paul’s account of his patellofemoral partial knee replacement surgery.
Book an assessment
CLICK HERE to book and appointment for an assessment of your knee.