The role of knee arthroscopy
There has been a lot written recently (particularly by non-experts) about the potential role of knee arthroscopy in degenerate knees, with a lot of confusing disinformation having been put out there by people who are not actually specialists in the field. On this page we try to dispel some of the misunderstandings and debunk some of the myths around the role of knee arthroscopy in degenerate / arthritic knees…
What does 'knee arthroscopy' mean?
‘Arthro’ means joint and ‘scopy’ means ‘to look‘ – and ‘knee arthroscopy’ simply means looking inside a knee joint with a camera. What it doesn’t tell you anything about is what’s actually wrong inside the knee (i.e. what the pathology / diagnosis might actually be) or what might actually be done inside the knee (i.e. what the specifics of the actual procedure are). Therefore, ‘knee arthroscopy’ is a term that absolutely cannot be bandied about as if it actually has any genuine meaning itself. Knee arthroscopy should not be thought of as an actual procedure: what it actually is is just a surgical approach that means that the inside of the knee can be inspected and probed in detail, actual diagnoses of specific intra-articular pathology can be confirmed, and surgical procedures (ranging from relatively minor to very major and complex reconstructions) can be performed minimally-invasively, through 5mm incisions rather than requiring full wide-open surgery.

‘Knee arthroscopy’ as a surgical approach therefore represents probably the biggest and best advance in surgical techniques of the knee in the last 50+ years!
What does knee arthroscopy involve?
Arthroscopic knee surgery is normally performed under a general anaesthetic as a day-case procedure (or overnight if the surgery is more complex and hence prolonged). It involves making 2 or more 5mm incisions at the front of the knee and inserting a camera and a probe into the joint. The whole of the inside of the knee joint can then be visualised and probed, which gives a lot more information than just an X-ray or an MRI scan.
What can knee arthroscopy do?
Arthroscopy plays an important role in the diagnosis of a large number of various potential pathologies that can occur within a knee joint, and this includes:
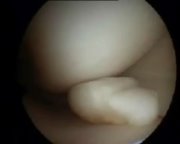
- meniscal tears,
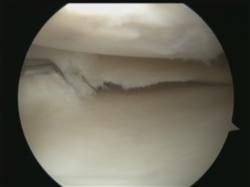
- fissures, flaps or defects in the articular cartilage on the joint surfaces,
- ACL tears (partial or total),
- osteochondral loose bodies,
- osteochondritis dissecans lesions,
- thickening / inflammation of the fat pad and
- medial and/or lateral and/or supra patellar plicae.
In terms of the potential surgical procedures that can actually be undertaken within a knee joint arthroscopically, the list (which again, is certainly not exhaustive) includes:
- meniscal trimming,
- meniscal repair,
- meniscal replacement (e.g. meniscal transplantation),
- radio frequency chondroplasty,
- abrasion chondroplasty,
- micro fracture,
- arthroscopic articular cartilage grafting,
- fixation of osteochondral / ossechondritis dissecans lesions,
- arthroscopic ACL repair,
- arthroscopic ACL reconstruction,
- washout of debris,
- removal of chondral / osteochondral loose bodies,
- trimming of the fat pad,
- excision of place,
- lateral release and
- synovectomy.
What a knee arthroscopy can’t do is to look deeper than just the joint surfaces (i.e. deep inside the bones themselves), and it cannot visualise structures outside of the joint capsule (the fibrous capsule that holds the joint fluid in), which means that you can’t see structures such as the MCL, the LCL, the posterolateral corner, the popliteal fossa or any of the musculature around the knee.
When is knee arthroscopy NOT appropriate?
A lot has been published over the last few years about the potential role of arthroscopic knee surgery in degenerate or arthritic knees, and a number of high-quality studies have confirmed that just ‘washing out’ an arthritic knee is a pointless exercise. However, this is nothing new, as all sensible knee surgeons already knew this years ago!
If there is fully-blown arthritis inside a knee (i.e. widespread bare bone), then just washing out the joint fluid along with any bits of cartilage debris is simply not appropriate, as it does not normally reduce symptoms significantly or delay the eventual requirement for knee replacement surgery. Unfortuantely, however, there is considerable misunderstanding of the terms ‘degenerate’ and ‘arthritic’…
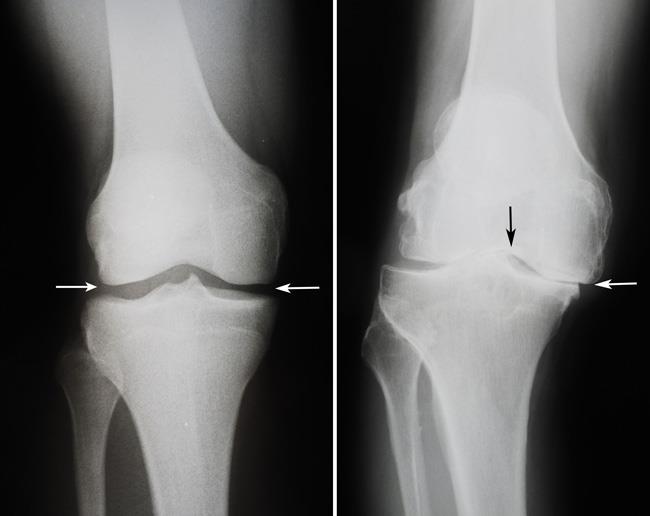
Osteoarthritis, or ‘wear and tear’ in a joint, is normally a slow gradual process whereby the articular cartilage gradually wears away. Initially it just wears thin, but if it wears away completely, leaving just widespread bare bone exposed in the joint, then this is normally referred to as ‘fully-blown arthritis’. The term ‘degenerate’, however, is extremely non-specific, and it could be used to describe a knee in a younger person with just minor early thinning of the articular cartilage, or it could be used to describe a fully-arthritic knee in an older person. The grade of arthritis is therefore important.
The grading system most widely used is the Outerbridge Classification, which grades knee degeneration into:
- Grade 1: softening of the cartilage
- Grade 2: fibrillation (roughening) of the cartilage
- Grade 3: fissuring (cracking) of the cartilage, or small patches of bare bone (<½ inch across)
- Grade 4: larger areas of full-thickness cartilage loss (exposed bare bone) >½ inch across.
Knee arthroscopy is rarely ever a suitable option in a patient with Grade 4 arthritis (i.e. ‘fully-blown’ arthritis with widespread bare bone exposed in the joint.
When can knee arthroscopy actually help?
If there are loose bodies causing ‘mechanical symptoms’ such as giving way or locking (like having loose stones in your shoe), then these can be removed. If there are rough or unstable edges or areas of articular cartilage damage in the joint, then these can be smoothed off and stabilised by arthroscopic radiofrequency chondroplasty. If there are symptomatic meniscal tears in a knee causing pain and/or mechanical symptoms (giving way / locking), then these can be trimmed smooth and stable (the likelihood of a degenerate meniscal tear actually being repairable is absolutely minimal). Any one or any combination of these procedures performed arthroscopically can significantly:
- reduce a patient’s symptoms,
- improve their function,
- help them keep their knee going for longer, and
- buy them additional time, delaying (though most probably not actually altogether avoiding) the eventual need for knee replacement surgery anyway, at some later stage.
So, if there are degenerative changes within a knee, but if the damage is not too far gone, then arthroscopic surgery can be fairly effective and it can be an appropriate treatment option in some patients’ knees.
CLICK HERE for further information about Dick Steadman’s study from Vale, Colorado, which showed that appropriately thorough arthroscopic knee debridement can buy patients an average of 7 years additional time before eventual knee replacement surgery.
Mr McDermott's explanation
How can I tell whether I'm an appropriate candidate?
If you want a proper opinion as to whether or not your knee might be suitable for any kind of arthroscopic surgery, then you need a full opinion from a proper expert — and the only genuine expert in the subject of knee surgery is a Consultant Orthopaedic Surgeon specialising specifically in knees!
A proper opinion will involve your consultant:
- taking a full and detailed history of your knee issues: what has happened to your knee in the past, what your symptoms are now, and how your sympotms are affecting your daily activities / work / exercising / sport (and this will include an assessment of your general health),
- performing a detailed clinical examination of your knee (and this will also include an assessment of your overall posture, gait and function),
- obtaining whatever relevant imaging might be required (if any arthritis is advanced, then simple X-rays may be all that might be required, but if any arthritis is only minor/early and/or if you want more detailed information, then you might need an MRI scan) (CLICK HERE for further information about knee imaging), and
- your consultant will then be able to have a detailed discussion with you about exactly what is actually wrong with your knee, followed by a discussion about the pros and the cons of each of the various potential treatment options that might be available and suitable for you.
For further information about Knee Assessments CLICK HERE.
Further information
Book an assessment
CONTACT US if you would like to arrange an appointment with a full assessment of your knee.