Biological Knee Replacement
‘Biological Knee Replacement’ is a term that probably orginated from Dr Kevn Stone, in San Francisco, who is a world-renowned pioneer in reconstructive knee surgery. What it refers to is replacing missing tissue in a damaged knee with grafts in order to repair or ‘regenerate’ the joint rather than resorting to replacing the joint with a metal and plastic prosthesis – i.e. an actual knee replacement.
Biological Knee Replacement is major complex surgery that is only performed by a very small number of surgeons worldwide, and by an even smaller number in the UK. Mr IanMcDermott has been developing, using and evolving the techniques for Biological Knee Replacement in the UK since 2010, and in 2014 he founded the UK Biological Knee Society as a study group for specialist knee surgeons wanting to promote the science and practice of reconstruction rather than replacement.
Biological Knee Replacement is only actually suitable for a relatively small proportion of patients. The surgery is complex and lengthy, with not-insignificant risks and requiring very slow and restrictive post-operative rehab afterwards. The medium-term success rates are ‘fair’, at about 80% at 5-year follow-up. The aim of Biological Knee Replacement is to reduce a patient’s knee symptoms, help maintain their function and help them keep their knee going for longer in order to try and delay (but most probably not actually avoid) the eventual need for knee replacement surgery anyway at some point in the later future.
Importantly, Biological Knee Replacement should be considered as salvage surgery only – it is not ‘restorative’ or truly ‘regenerative’, and it does not ‘grow you a new knee that is as good as normal.
What does Biological Knee Replacement involve?
The meniscal cartilage shock absorbers in the knee can and do often tear. About 25% or so of meniscal tears in younger patients (<40) can be repairable (CLICK HERE to read about meniscal repair), which unfortuantely means that 75% are not repairable. Degenerate meniscal tears (tears that develop in older patients (>40) through ‘wear and tear’ are rarely if ever repairable. If a meniscal tear is symptomatic enough to justify intervention, then a knee arthroscopy is normally required, and if the tear is not repairable then it will end up being trimmed, with a partial mensicectomy. The more a meniscal cartilage is damaged, and the more tissue ends up having to be trimmed / removed, then the less of a shock absorber is left in that side of the knee, and hence the faster the rate of wear and tear will be on the articular cartilage on the joint surfaces… which significantly increases the risk of subsequent arthritis in that knee in the longer-term future.
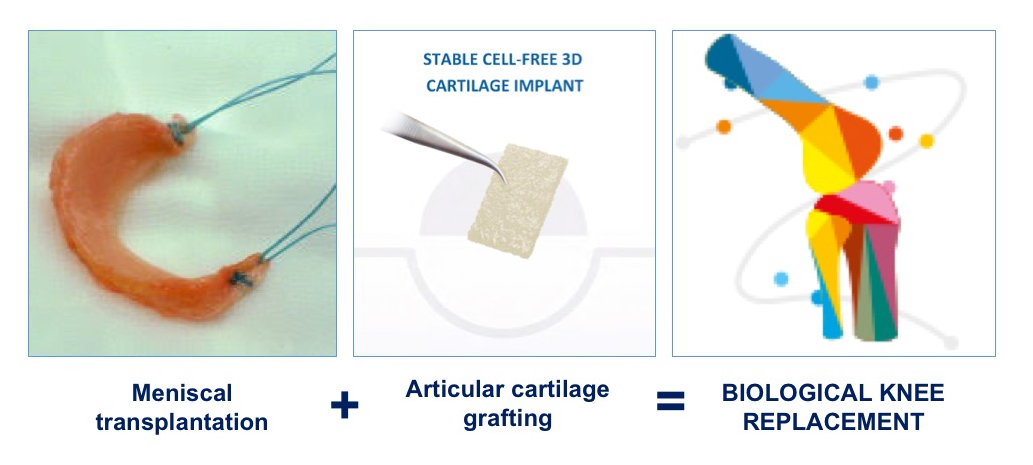
So, if most or all of a meniscus is missing in your knee and if you are starting to develop progressive symptoms and signs of articular cartilage wear and tear / degeneration, then the missing meniscus can be replaced by meniscal allograft transplantion. For futher information about meniscal allograft transplantation CLICK HERE.
Importantly, however, if the articular cartilage in a knee joint is already too badly damaged, and in particular, if there is full-thickness cartilage loss with actual bare bone exposed, then the rough hard bare bone surfaces will simply abrade a meniscal allograft and the meniscal transplant will be far more likely to fail.
Therefore, if a patient has full-thickness articular cartilage loss as well as meniscal deficiency, then it is possible to perform articular cartilage grafting at the same time, in addition to the meniscal transplant. CLICK HERE to read more about articular cartilage grafting.
Similarly, if a patient has articular cartilage grafting surgery but there is not a normal or near-normal meniscus in that compartment of the knee to protect the new cartilage graft, then the articular cartilage graft will be far more likely to fail.
Therefore, if there is articular cartilage loss in a compartment of a knee and meniscal loss, and if you want to try and get the best possible long-term result, then there is a strong argument for performing articular cartilage grafting and meniscal allograft transplantation together, at the same time – and this is what is referred to as Biological Knee Replacement.
In addition to this, if there is a torn or slack ligament in the knee, with joint instability, then for the Biological Knee Replacement to work one also has to reconstruct the ligament as well. CLICK HERE to read about ligament reconstruction.
Finally, if there is malaligment on the joint then this also has to be corrected too, which may require a realignment osteotomy. In younger patients once might consider combining the realignment osteotomy surgery with the Biological Knee Replacement, at the same time, although this then makes the surgery even more major and complex. Alternatively, one might perform the realignment osteotomy surgery first, then wait a few months for the patient to recover, before then potentially proceeding with the Biological Knee Replacement surgery later, as a second-stage procedure. In older patients (closer to 50), it can often be more appropriate to perform just the realignment osteotomy surgery only, as a sole procedure.
Mr McDermott's explanation
Am I too old?
Most surgeons tend to agree that the age cut-off for Biological Knee Replacement surgery is probably 50. This is not surgeons being ‘ageist’! – it’s simply because the older you are then the poorer your healing ability will be and the less able you will be to cope with major complex surgery and the extensive post-op rehab that would be required afterwards… and hence the lower the likelihood would be of you achieving a good outcome.
In addition to this, the older you are then the more likely you are to be either in or at least close to the age range where artificial joint replacement surgery is more acceptable and appropriate.
CLICK HERE to read about the timing of when artificial joint replacement surgery might actually be appropriate.
How can I tell whether I might be a suitable candidate?
If you want to know whether or not your knee might potentially be suitable for Biological Knee Replacement surgery, then this requires a proper, full, detailed assessment from a specialist knee surgeon who actually undertakes this kind of surgery.
If you have already had X-rays that have shown that you already have fully-blown arthritis in your knee, then you are very unlikely to be a suitable candidate for reconstructive surgery. However, if you do want a proper opinion then this requires:
- a face-to-face assessment, with your surgeon taking a full history of your issues,
- a proper hands-on clinical assessment,
- a full set of X-rays, including long-leg weight-bearing alignment X-rays and
- a decent quality recent / up-to-date MRI scan of your knee.
Your surgeon might also recommend undertaking just a knee arthroscopy as well, first – in order to evaluate the joint in more detail and also to tidy-up any damage in the joint at the same time (and in some people, just the knee arthroscopy alone might end up being sufficient and all that the patient might actually need for the time-being).
Tina's Biological Knee Replacement surgery
Tina very kindly agreed to be interviewed to share her experiences of her Biological Knee Replacement surgery…
Book an assessment
CONTACT US if you would like to arrange an appointment with a full assessment of your knee.