Total knee replacements
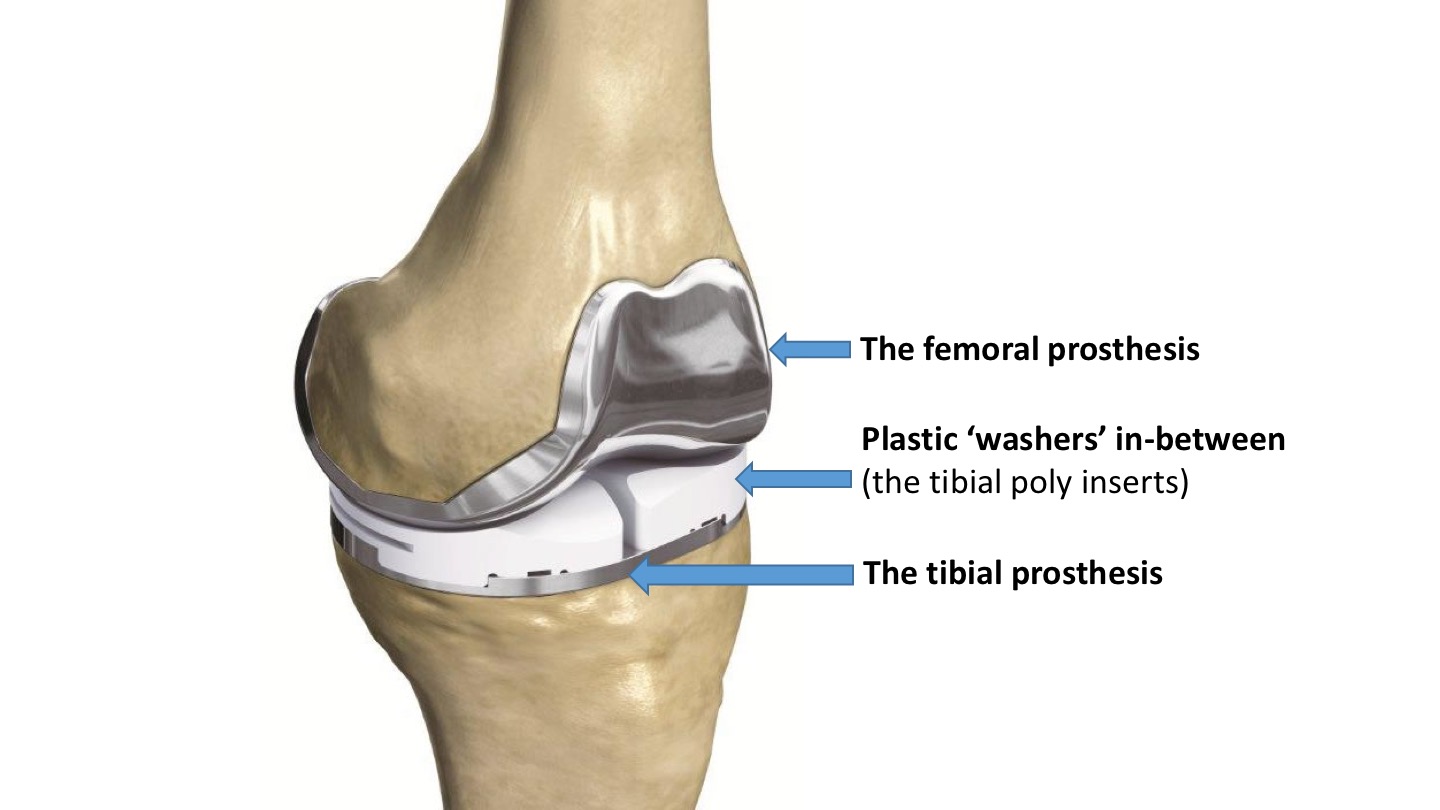
‘Knee replacement’ really means ‘knee resurfacing’, and knee replacement surgery actually involves replacing the surfaces of the bones with metal surfaces, with plastic ‘washers’ in-between.
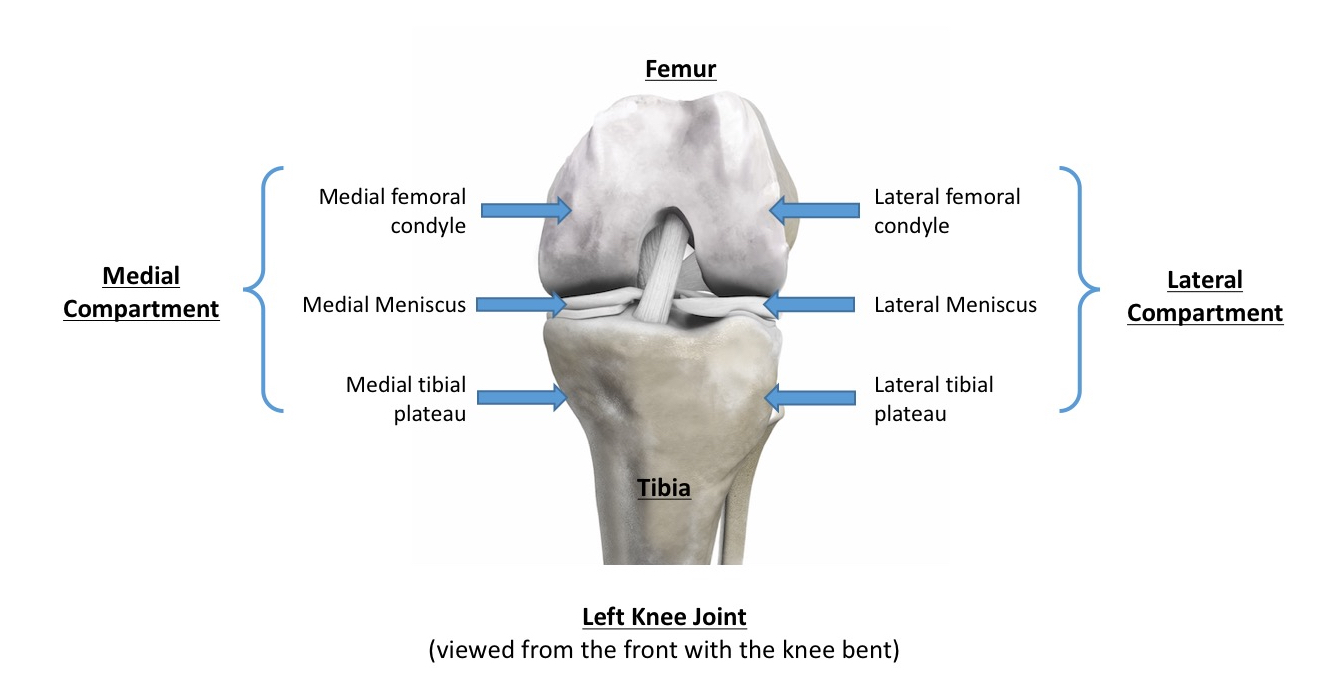
Orthopaedic Surgeons refer to the knee as having 3 ‘compartments’. In reality, the knee joint is just one single compartment full of joint fluid (synovial fluid) that is contained within a fibrous capsule. However, it helps to refer to different areas within a knee as compartments, with:
- the medial compartment = on the inner side of the knee, and it includes the inner side of the end of the femur (the medial femoral condyle), the inner side of the top of the tibia (the medial tibial plateau) and the medial meniscus (the meniscal cartilage ‘shock absorber’) sitting in-between,
- the lateral compartment = on the outer side of the knee, and it includes the outer side of the end of the femur (the lateral femoral condyle), the outer side of the top of the tibia (the lateral tibial plateau) and the lateral meniscus sitting in-between, and
- the patellofemoral compartment = at the front of the knee, and this refers to the articulation between the back of the kneecap and the V-shaped groove (the trochlear groove / the trochlea) in the middle of the front of the end of the femur.
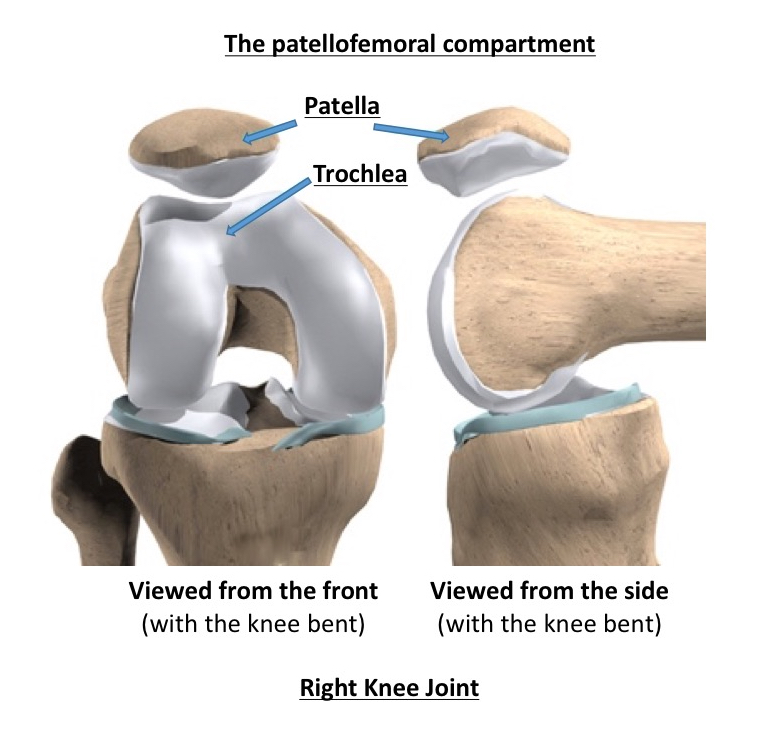
When both the medial and the lateral compartments +/- the patellofemoral compartment are replaced / resurfaced, then this is what is referred to as a total knee replacement.
The 'prostheses'
A knee replacement consists of two separate ‘prostheses’:
- the femoral prosthesis is the metal implant used to resurface the end of the femur
- the tibial prosthesis is the metal implant used to resurface the top of the tibia.
The space in-between the two metal prostheses is filled with a rock-hard plastic spacer, which is made of ultra-high molecular weight polyethylene (UHMWPE).
Cemented vs cementless
In most cases, the metal prostheses are fixed to the cut and contoured bone surfaces using special polymethylmethacrylate bone cement. Some makes of prosthesis are cementless, in which case they are simply press-fit, with the metal on the back of the prosthesis being textured (rough) and covered in hydroxyapatite, with the bone simply growing onto the surface of the metal with time.
Most surgeons agree that in general, it is best to use cement to fix the tibial prosthesis, as this tends to give the best results. Studies have show, however, that on the femoral side there is little if any difference in outcomes between cemented vs cementless prostheses.
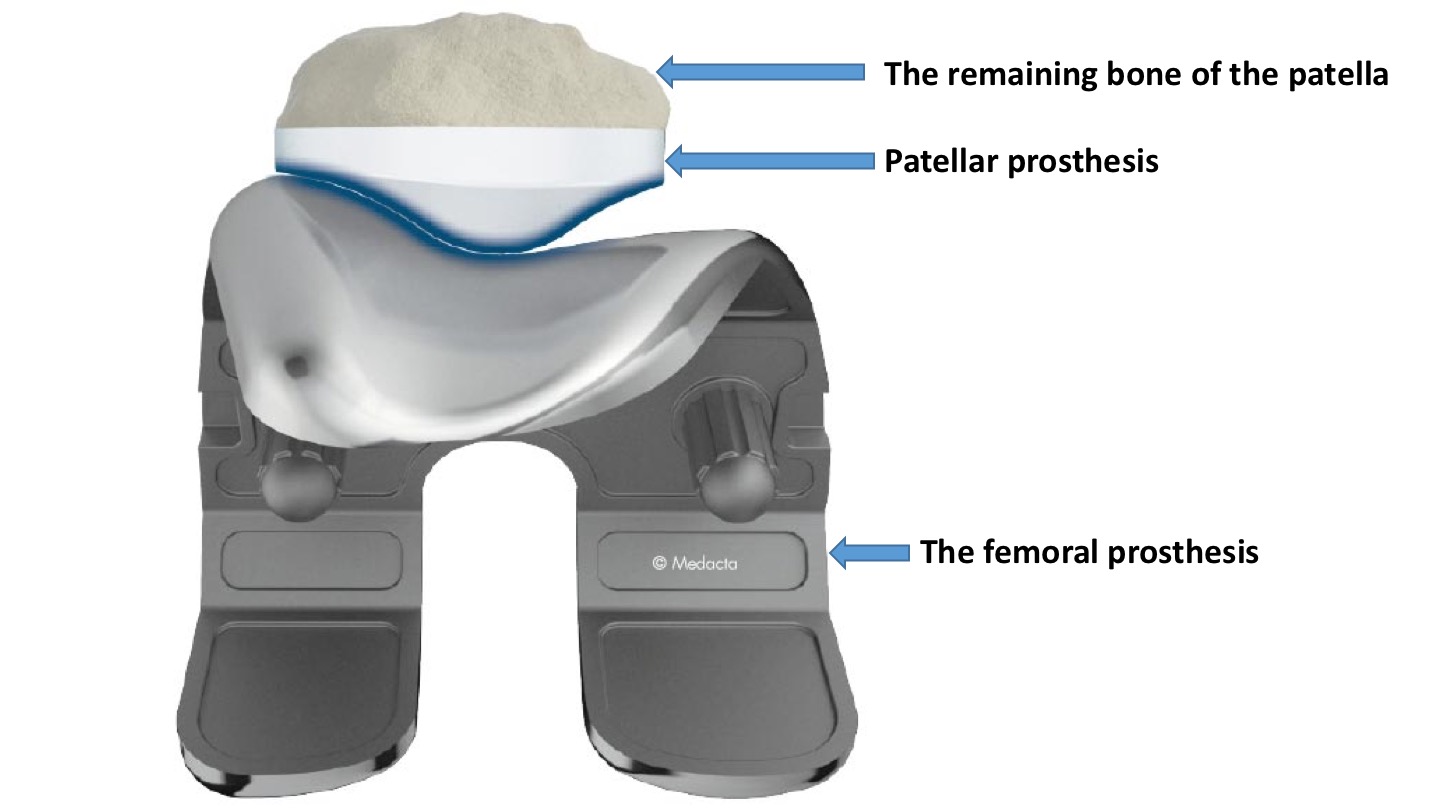
Patellar resurfacing
The question as to whether or not one should also resurface the patella when one performs a total knee replacement is slightly contentious…
If you do have your patella resurfaced, the this involves sawing off the back surface of the patella, where the articular cartilage is (or was) and cementing a plastic domed ‘button’-type prosthesis in place.
Different surgeons seem to have different opinions and approaches to patellar resurfacing:
- some surgeons always resurface the patella
- some surgeons never resurface the patella, and
- some are ‘selective resurfacers’, and resurface the patella only if the patella looks significantly damaged / arthritic.
Some types of knee replacement seem to give good results whether the patella is resurfaced or not. However, in others, it has been shown that better results are obtained if the patella is always resurfaced.
The surgeons who don’t resurface the patella (or who only sometimes resurface it) state that this reduces surgical time and that it reduces the chances of complications arising from the patellar resurfacing itself (such as patellar fracture or loosening of the patellar prosthesis/button – although these are extremely rare).
The surgeons who always resurface the patella do so specifically to avoid A) ongoing pain at the front of the knee post-operatively, from residual arthritic damage to the kneecap, and B) to avoid the risk of one potentially having to go back in later and perform a second operation, with delayed patellar resurfacing if the patient does continue to suffer with ongoing anterior knee pain.
My personal approach is that I always resurface the patella (Mr Ian McDermott)
Cruciate-retaining vs Posteriorly-stabilised
When a knee replacement is performed, the medial and lateral collateral ligaments are always preserved. This gives varus / valgus (sideways) stability to the joint.
The anterior cruciate ligament (ACL), however, is always removed. This is because the normal ACL attaches towards the front of the middle of the top surface of the tibia (the tibial plateau), and this is always cut away and replaced with the tibial prosthesis. The reasons that this is not actually a problem are that:
- the top surface of the tibial poly (plastic) insert is curved, with a slight lip at the back, and this shape naturally causes the tibial not to slide forwards whilst the joint is loaded, and
- knee replacements are just not designed for impact / pivotting type exercise / sport. A knee joint can cope perfectly well with in-line activities, such as walking, cycling, cross-country skiing or even running in straight lines. However, the ACL gives stability to the joint for pivoting type activies (i.e. changing direction on a bent knee at speed), e.g. football, basketball, racket sports etc. If you want your knee replacement to last as long as possible then you should protect it, not ‘pound’ it. Therefore, you shouldn’t actually perform impact-type exercise / sport… and a knee replacement without an ACL present should be perfectly stable for all daily activities and for exercise and gentle sport that does not involve pivoting.
The posterior cruciate ligament (PCL), on the other hand, is normally retained with most standard knee replacement prostheses.
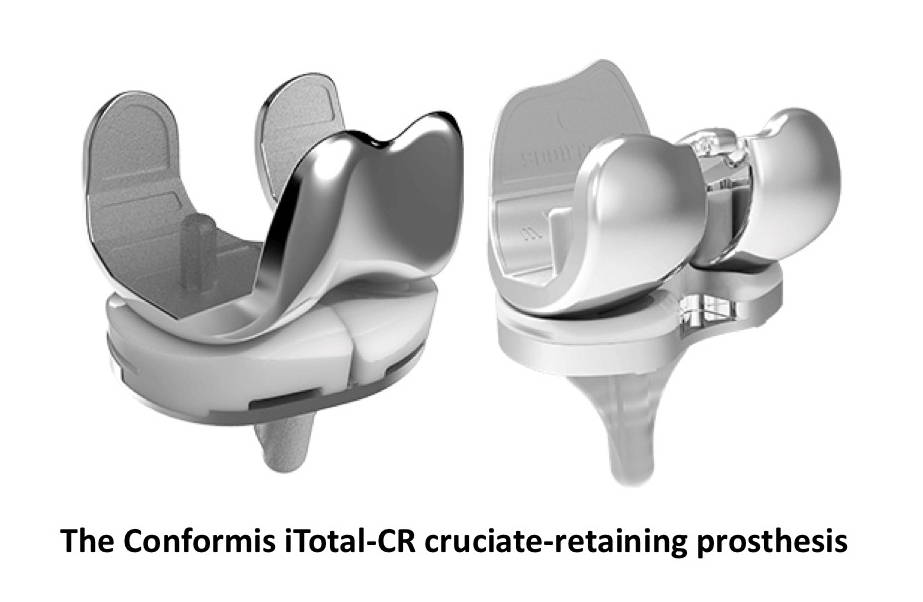
If the PCL is retained, then this is what is meant by a ‘cruciate retaining’ (CR) knee replacement.
If a knee has significant deformity (especially valgus deformity) and/or more bone loss than normal, and/or the joint is particularly stiff (with either very reduced flexion or a large fixed flexion), and/or if the joint is more unstable than usual… then your surgeon might opt to remove the PCL, which allows for easier corrections of greater issues. To give better stability, one then has to use a ‘posteriorly stabilised’ (PS) knee prosthesis, where there is a post in the middle of the tibial poly spacer that engages against a bar towards the back of the femoral prothesis, which gives stability against the tibial wobbling backwards.
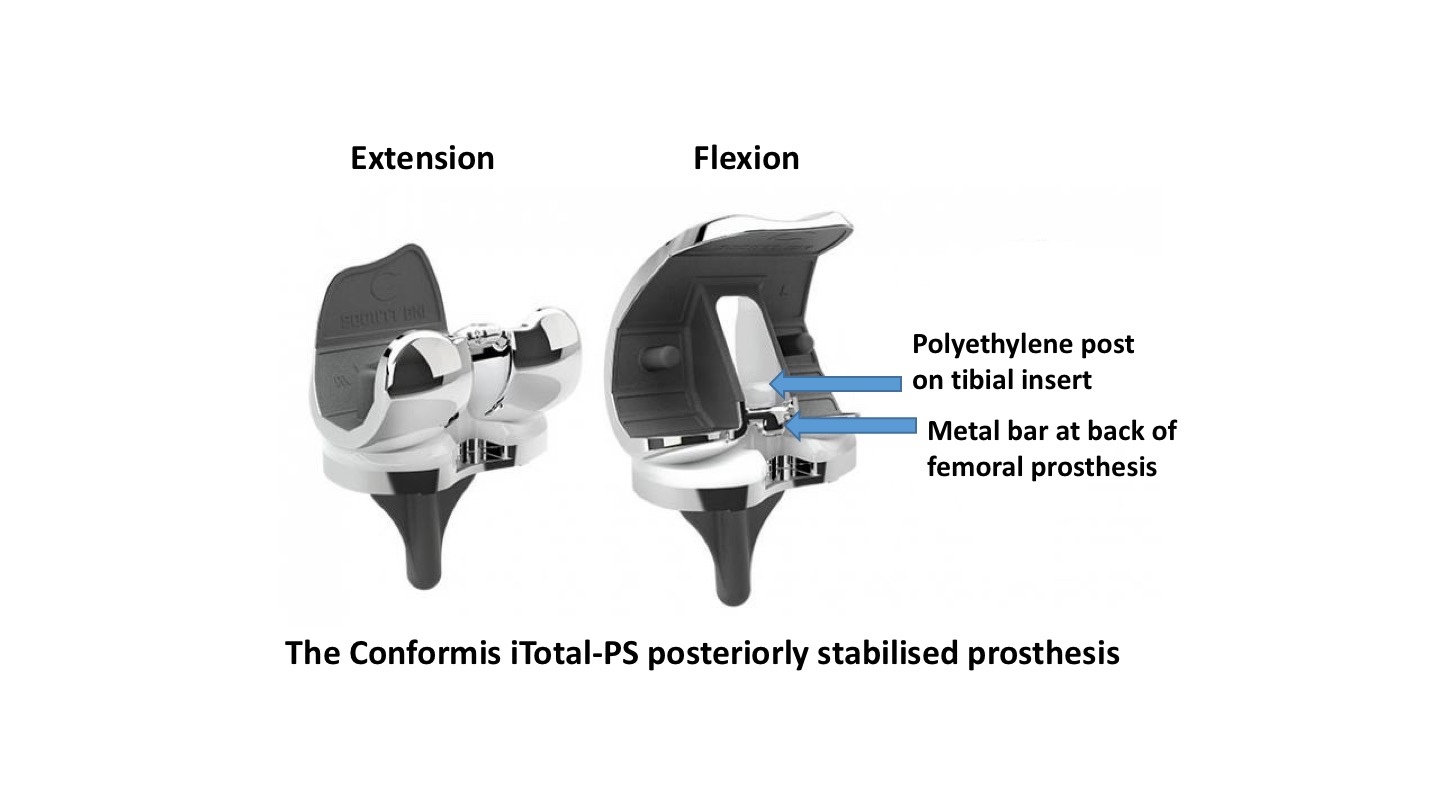 CLICK HERE for further information about the Confomis iTotal-PS posteriorly-stabilised custom-made knee replacement prosthesis.
CLICK HERE for further information about the Confomis iTotal-PS posteriorly-stabilised custom-made knee replacement prosthesis.
